Abstract
BackgroundIdiopathic intracranial hypertension (IIH) is a syndrome of elevated intracranial pressure of unknown etiology. Unilateral or bilateral transverse sinus (TS) or transverse-sigmoid junction stenosis is present in about 30%–93% of these patients. There is an ongoing debate on whether venous sinus stenosis is the cause of IIH or a result of it. The subset of IIH patients who continue to have clinical deterioration despite maximum medical therapy is termed as “refractory IIH.” Traditionally, cerebrospinal fluid diversion surgeries (ventriculoperitoneal shunt and lumboperitoneal shunt) and optic nerve sheath fenestration (ONSF) were the mainstays of treatment for refractory IIH. In the last decade, venous sinus stenting (VSS) has emerged as a safe and effective option for treating refractory IIH patients with venous sinus stenosis. Through this study, we want to share our experience with venous stenting in refractory IIH patients with venous sinus stenosis associated with a significant pressure gradient (≥10 mm Hg).
MethodsRetrospective chart review of all the patients diagnosed with refractory IIH who underwent VSS or angioplasty at our comprehensive stroke
center from November 2016 to March 2019.
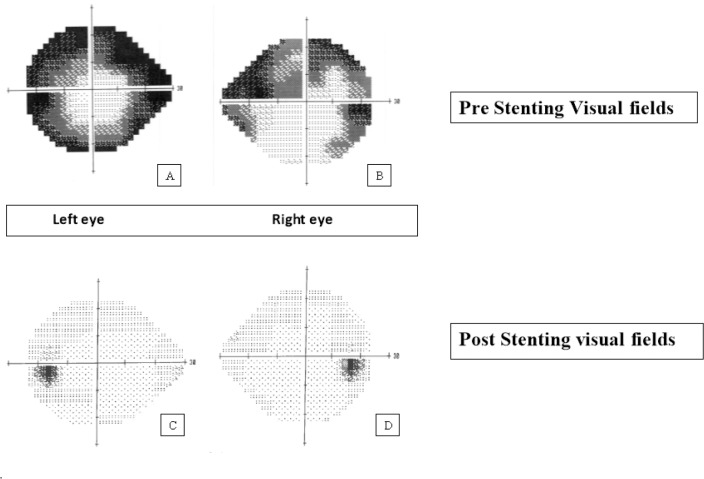
ResultsA total of seven refractory IIH patients underwent VSS or angioplasty within the specified period. The mean age was 39 years. Eighty-five percent of the patients were women (n = 6). The mean body mass index (BMI) was 37 kg/m2. Headache was the most common symptom (85%, n = 6) followed by transient visual obscurations (71%, n = 5) and pulsatile tinnitus (57%; n = 4). All patients had papilledema. Fifty-seven percent of patients (n = 4) had impaired visual field. Mean lumbar opening pressure was 40.6 cm H2O (SD = 9.66; 95% CI = 33.5—47.7). All patients were on maximum doses of acetazolamide ± furosemide. Six patients (85%) had dominant right transverse-sigmoid sinus. Fifty-seven percent of the patients had severe right transverse ± sigmoid sinus stenosis (n = 4) and the rest (43%) had bilateral TS stenosis (n = 3). Prestenting mean trans-stenosis pressure gradient was 18 mm Hg (SD = 6.16; 95% CI = 13.43–22.57). Six patients (85%) were treated with TS stenting and one (15%) with only angioplasty. Poststenting mean trans-stenosis pressure gradient was 4.8 mm Hg (SD = 6.6; 95% CI = −0.1–9.7). All patients were able to come off their medications with significant improvement in neurological and ophthalmological signs and symptoms. No procedure-related complications occurred.
ConclusionTS stenting ± angioplasty is a safe and effective means of treating refractory IIH with venous sinus stenosis associated with a significant pressure gradient (≥10 mm Hg).

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright (c) 2022 Journal of Vascular and Interventional Neurology